Diabetes
A to Z of diabetes and hormones for you
A1C Test
If you are talking with someone about diabetes, you may hear the term “A1C.”
What exactly does A1C mean?
How important is A1C for diabetes management?
An HbA1C blood test is one of the most important tests to determine your overall diabetes control. It reflects overall control of diabetes and important for how well you will be in future.
A1C
The A1C goal for most people with diabetes is less than 7%. Your goal may be different, however, so it’s important to talk with your doctor about the target that’s best suited for you.
 The A1C, also known as a glycohemoglobin or hemoglobin A1C, provides a clear picture of your average glucose control for the past three months. The A1C measures the glucose that binds to hemoglobin in your red blood cells. The higher the glucose levels in your blood, the more glucose binds to the hemoglobin, and thus the higher your A1C level will be. Red blood cells are renewed every 120 days. By measuring the percentage of hemoglobin molecules that have glucose attached to them, you and your doctor can get an average of your glucose over three months.
The A1C, also known as a glycohemoglobin or hemoglobin A1C, provides a clear picture of your average glucose control for the past three months. The A1C measures the glucose that binds to hemoglobin in your red blood cells. The higher the glucose levels in your blood, the more glucose binds to the hemoglobin, and thus the higher your A1C level will be. Red blood cells are renewed every 120 days. By measuring the percentage of hemoglobin molecules that have glucose attached to them, you and your doctor can get an average of your glucose over three months.
The A1C test is done every three months. It does not require fasting, and can be done any time of day.
Why is the A1C test essential for diabetes management?
It gives you an overall picture of your diabetes, rather than a reflection of what is happening in one day, and helps you evaluate your diabetes care and make changes. An A1C test can help you manage your diabetes by:
It’s helpful to remember that the closer you get to your goal, the better you’ll feel today and tomorrow. According to Dr Noel Somasundaram ‘we recommend that patients aim for an A1C value of less than 7 percent’. This has to be done without increasing your risk for developing hypoglycemia ( low blood glucose).
The higher your A1C, the greater your risk for developing complications, such as heart attacks, strokes, kidney disease, and neuropathy, foot ulcers, and amputations. To help lower your risk for diabetes complications, keep your glucose levels in your target range by self-monitoring and making adjustments with medicine (insulin, tablets, or both), weight control, food control, and regular physical exercise.
What Do You Do if Your A1C Is above 7% or above Your Individual Target?
If your A1C is above target, it tells you that your diabetes treatment plan needs a change. This could mean that you need to develop a new plan to control your diabetes. By making an appointment to consult you can decide which medications best suit you as well as talk about your meal plan, and exercise. Most often you require new medications and change in diet and exercise. You may have to check your glucose at home. Set up an appointment to discuss the results with your doctor to ensure that you control your diabetes.
Blood Glucose
What is High Blood Glucose?
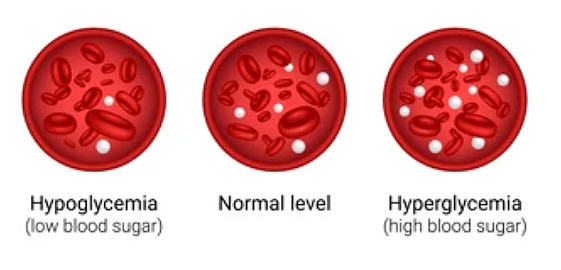
People who do not have diabetes usually have fasting plasma blood glucose levels that run under 90 mg/dl.
In diabetes patients controlling blood glucose values and keeping them close to normal as possible will help you safely achieve life without complications of diabetes. In general, high blood glucose, also called ‘hyperglycemia’, is considered “high” when it is 140 mg/dl. Ask your doctor what he thinks is a safe target for you for blood glucose before and after meals.
If your blood glucose runs high for long periods of time, this can cause significant problems for you long-term; you are at increased risk of complications, such as eye disease, kidney disease, heart attacks and strokes and amputations. High blood glucose can pose health problems in the short-term as well such as infections and coma in some patients. Your treatment plan may need adjustment if the blood glucose stays over 180 mg/dl for 3 days in a row. It is important to aim to keep your blood glucose under control and treat hyperglycemia when it occurs.
What are the symptoms of high blood glucose?
- Increased thirst
- Increased urination
- Dry mouth or skin
- Tiredness or fatigue
- Blurred vision
- More frequent infections
- Slow healing wounds
- Unexplained weight loss
- Lack of energy
What causes high blood glucose?
- Too much food
- Too little exercise or physical activity
- Not taking medications and insulin
- Not being regular with medications and insulun
- Insulin that has become ineffective after being exposed to extreme heat or freezing cold
- Stress, illness, infection, injury or surgery
- A blood glucose meter that is not reading accurately
What should you do for high blood glucose?
- Be sure to drink plenty of water. It is recommended to drink a minimum of 8 glasses each day.
- If your blood glucose is 250 or greater and you are on insulin, check your urine for ketones. If you have ketones, contact your doctor.
- Ask yourself what may have caused the high blood sugar, and take action to correct it. Ask your doctor if you are not sure what to do.
- Try to determine if there is a pattern to your blood glucose levels.
- Check your blood glucose before meals 3 days in a row.
- If greater than your target level for 3 days, a change in medication may be needed.
- Contact your doctor or adjust your insulin dose.
- Contact your doctor if you are currently using diabetes tablets only.
Determine why your blood glucose is high
Ask yourself the questions outlined below. The answers will give you the information you need to determine what to do about the hyperglycemia.
If your answers to the questions are yes, follow these suggestions.
Causes | Ask These Questions | Take Action |
Food | Have you increased the food? | You may need to review the amount of food you take, particularly the carbohydrates, fruits and sweets. If you think your eating pattern is changing, your medication or exercise plan may need to change. |
Activity | Have you decreased or stopped your usual exercise? | Physical activity and exercise is key to blood glucose control. Ask your doctor and his team about starting a program. |
Medication | Have you been taking the prescribed doses? | Take the right dose at the right time. If you have any questions ask a your doctors team. Check the expiration date on the package. |
Monitoring | Is the drop of blood too small? | Learn how to clean the meter. |
Illness, infection, injury and surgery | Are you feeling well? | Follow sick day rules. |
Diabetes, High Blood Pressure and Kidney Disease



High blood pressure (hypertension) is one of the principal causes of kidney disease and heart attack and stroke. When blood pressure is high, there is a large amount of tension inside the blood vessels that leads to damage. These vessels may constrict (“close off”), which can cause a heart attack, stroke, or kidney failure.
High glucose and high cholesterol can also damage blood vessels. Thus people with diabetes who also have hypertension are at especially high risk for blood vessel damage. It usually takes years for blood vessels to completely constrict, and damage to blood vessels can be slowed down or somewhat reversed with treatment.
The ABC of diabetes
By controlling you A- A1C, B- blood pressure and C-Cholesterol you can prevent complications of diabetes.
Diagnosis
Diagnosis of high blood pressure can only be done by having your blood pressure measured regularly. Usually, there are no obvious symptoms that indicate you have high blood pressure. If you have diabetes, the blood pressure is considered high if it is more than 130/80.
Your blood pressure should be measured on multiple occasions, as blood pressure can vary throughout the day and it is normal to have occasional readings greater than 130/80. Blood pressure generally peaks in the middle of the day, and is lowest at night while you are sleeping. It is best to take blood pressure from the left arm, if possible, and should be taken after you have rested for 5-10 minutes. Your left arm should rest comfortably at heart level.
Your doctor may ask you to check your blood pressure at home and record the readings as part of your blood pressure management.
Treatment
There are multiple ways to control your blood pressure. The first step is lifestyle changes.
Lifestyle Changes
Your diet and lifestyle can directly affect blood pressure. For example, too much sodium (salt), alcohol, or caffeine intake may increase your blood pressure. Your weight also affects your blood pressure. Increased weight leads to fluid retention, and the extra fat releases hormones that can make blood pressure rise. Excess weight also causes the heart to work harder. Routine exercises can speed-up weight loss.
Exercise can lower your systolic blood pressure – the top number in a blood pressure reading – by upto 4 to 9 mmHg. Some people can even reduce their need for blood pressure medication with exercise. Regular exercise also makes your heart stronger, making it able to pump more blood with less effort. Even if you do not have high blood pressure, regular exercise can help prevent it from rising as you age.
Weight loss, lowering sodium, alcohol and caffeine in your diet, in addition to decreasing stress, while increasing exercise are all an important parts of blood pressure control.
Medications
It is not uncommon for one to need one or several medications to achieve good blood pressure control. Many research studies have shown that you may need to take several medications to get your blood pressure to a goal of less than 130/80. You and your doctor can decide what are the best medications for you.
Gestational Diabetes
Managing Diabetes During Pregnancy
 Imagine wanting to get pregnancy and bring discouraged from doing so. About 25 years ago, this was the case for many women with diabetes. However, with recent advances in diabetes management and careful planning, the chances of having a successful pregnancy are excellent! Talk to us about having a successful childbirth despite diabetes.
Imagine wanting to get pregnancy and bring discouraged from doing so. About 25 years ago, this was the case for many women with diabetes. However, with recent advances in diabetes management and careful planning, the chances of having a successful pregnancy are excellent! Talk to us about having a successful childbirth despite diabetes.
It’s all about planning
Preconception Planning
If you have diabetes and are thinking about becoming pregnant, it is recommended that you start preparing about 6 months prior to conception. The most important thing to do before conception is to have your diabetes in good control and to learn how to continue managing your diabetes during pregnancy.
Once you’ve decided you want to become pregnant, you should make an appointment with your endocrinologist (a diabetes physician specialist) to review your health status and pregnancy plans. If you don’t have an endocrinologist, your primary care provider can refer you to one.
In addition to an endocrinologist, there are other who can help you during your pregnancy: an obstetrician, of course; but other members of your healthcare team my include a dietitian who focus on the management of diabetes. You may be referred to other specialists by your endocrinologist. While you will be the one in charge of your pregnancy, it is still necessary to have a medical team as well as loved ones to support you during this time.
You will need to meet with your obstetrician more frequently than a woman without diabetes. These visits may include ultrasounds to determine fetal growth and development and other laboratory tests. It is important to know that you will be scheduling a number of visits with your team during your pregnancy.
Dr Noel Somasundaram recommends the following goals and medical assessments before pregnancy:
- Fasting and pre-meal blood glucose: 80-110 mg/dl
- Blood glucose one hour after meal: 100-130 mg/dl
- A1C, as close to 6% as possible without hypoglycemia
- Blood pressure below 130/80 mm Hg (if you are taking medication for your blood pressure, the medicine has
- to be reviewed to make sure that it is safe for use when pregnant)
- Review of diabetes and obstetrical history
- Eye evaluations to screen for and discuss risks of diabetic retinopathy
- Renal, thyroid, gynecological and sometimes cardiac evaluations
The critical stages of development for a baby begin within the first 4 weeks, which is often when a woman can’t even tell she is pregnant. Even so, during this time the baby’s spine and organs are formed. This is why it is important to keep your blood glucose levels in the target range prior to conception in order to help reduce the risk of harm to your baby. Checking your blood glucose three times daily and having an A1C test will help tell you if you’re staying on track. During your pregnancy, your A1C is checked every month. Chart your blood glucose values and send them periodically to your endocrinologist for review.
If You Are Already Pregnant
More than half of all pregnancies are unplanned. If you fall into this category and discover that you are pregnant, it’s important that you schedule an appointment with your endocrinologist and your obstetrician right way.
Glucose Management in Pregnancy
For the health of you and your baby, it’s important to achieve the best possible blood glucose control, while avoiding hypoglycemia. The table below lists the recommended glucose goals during pregnancy.
Measurement | Goal |
Fasting and before meals | 70-95mg/dL |
1 hour after meals | 100-129mg/dL |
A1C | Below 7% and as close to 6% as possible |
Urine Ketones | Negative |
Taking Insulin
Women with type 1 diabetes must take insulin to manage their diabetes, and during pregnancy will find that the amount of insulin that they need will increase. Because diabetes pills have not been approved by the Food and Drug Administration (FDA) for use during pregnancy, woman with type 2 diabetes may also need to take insulin during their pregnancy, as well. As the pregnancy progresses, more insulin may be needed to compensate for the placental hormones that raise blood glucose. By the end of your pregnancy, you may need 2-3 times more insulin than you needed before pregnancy. Your healthcare team will work with you to find the insulin regimen that best meets your needs.
Nutrition
The food you eat during pregnancy not only helps your baby grow, but it also has an effect on your blood glucose levels and for this reason, a dietitian is an important member of your healthcare team. Part of a dietitian’s job is to provide you with a meal plan than takes into account you and your baby’s nutritional needs, your lifestyle, and the foods you like and dislike. A dietitian will also be able to tell you which foods are important to eat and which ones are best to omit during pregnancy in addition to helping you gain the appropriate amount of weight for each 3-month trimester of your pregnancy.
Activity
Exercise is an important part of managing diabetes, and is recommended as a safe therapy for managing diabetes in pregnancy. Women who are active for at least 5 days each week and who do aerobic and strength training exercises are more likely to have an easier pregnancy. Blood glucose is affected by exercise during pregnancy. Checking blood glucose around exercise is important to keep both you and your baby safe.
It’s okay to continue most activities during your pregnancy; however, it is best to check with your healthcare team, especially if the activity is strenuous such as skiing or hot yoga.
Gestational Diabetes
Gestational diabetesis the term used when diabetes is diagnosed during pregnancy. It usually develops between the 24th and 28th week of pregnancy and affects anywhere from 6-9 percent of all pregnancies. The treatment, blood glucose monitoring, scheduled office visits, meal planning, activity and medication are similar to the guidelines described above. Your healthcare team will help develop a specific care plan for you. It is very important that, once you deliver your baby, you schedule a follow-up appointment for laboratory testing and healthcare review with your team because women who have gestational diabetes are at risk for developing type 2 diabetes later on in life.
Postpartum (After Pregnancy)
With careful diabetes management, women can and do have successful pregnancies and healthy babies.
After your baby is born and you have seen your obstetrician for a follow-up visit, plan a healthcare check-up visit with your endocrinologist to review your blood glucose control, possible medication changes and weight management.
Sick Day Rules
Advice for when you are sick
People with diabetes have been identified as one group that may face greater risks of complications when dealing with COVID-19. With that in mind, Dr Noel Somasundaram has prepared these guidelines for adults with diabetes who may find themselves dealing with any kind of viral symptoms.
What to do if you are feeling sick and have diabetes?
On days when you are sick, your glucose levels can go high even if you are eating less than you usually do.
Having any of these conditions below can cause a “sick day” and may make your glucose levels go up.
-
- Common cold
- Influenza (“flu”)
- Nausea, vomiting, diarrhea
- Infection
- Surgery
- Dental work
- Stress
- Injury
Steps to take when you are feeling sick
Untreated high glucose levels can lead to more serious medical problems, so it is important to have a plan. The following are the steps to follow when you are sick.
-
- Always take your diabetes medicine unless your doctor tells you not to. Even if you are unable to eat your usual meals, you may need to take your insulin or diabetes pills. If your glucose is over 250 for two readings in a row, call your doctor because you may need a change in your medicine.
- Monitor your glucose more often. Monitor your glucose 4 times per day for mild illnesses (like a cold) or every 3 to 4 hours for more severe illnesses (like the flu). You will need to monitor your glucose more often when you are ill is important because it can get high quickly. You will not always know if your glucose is by how you are feeling.
- Check for ketones when your glucose is over 250 mg/dl if you have type 1 diabetes.
- Drink plenty of fluids. Drink at least 2 to 3 liters of fluids per day to prevent dehydration.
- If you are unable to eat solid food, take sugar free drinks for one hour (king coconut water, soda, water, tea) and liquids that contain sugar (fruit juice, regular soda) for the other hour.
- Rest – Do not exercise.
- It would be helpful to have a support person available.
When to call your doctor
There may be times when you feel very sick or just aren’t sure what to do. It’s best to be on the safe side and call your doctor, especially if you:
-
- Have signs of dehydration such as dry mouth, cracked lips, sunken eyes, skin that is flushed and dry or weight loss
- Have a fever of 101ºF or higher
- Have persistent nausea or vomiting or are unable to keep fluids down
- Have persistent diarrhea
- Have persistent abdominal pain
- Have rapid, shallow breathing
- Have glucose levels over 250 mg/dl for more than two readings with or without ketones
- Have persistent moderate-large ketones
- Have persistent low glucose
In these scenarios you may have to go to the hospital. Remember to bring your insulin and prescriptions to avoid dosing errors.
Monitor your glucose 4 times per day for mild illnesses (like a cold) or every 3 to 4 hours for more severe illnesses (like the flu).
Monitoring Diabetes
Home Blood Glucose Monitoring, Hemoglobin A1c Testing, and Fructosamine Tests
There are many ways to monitor your diabetes and your diabetes control. Daily information is valuable to make decisions in the moment, while tests like A1c and Fructosamine provide an overall idea of control over a longer time period. Hemoglobin A1c tests tell you and your endocrinologist what your glucose control has been on average over the past three months. The fructosamine test is similar to an A1c but measures your average glucose over two weeks. Each type of test has its advantages and usefulness.
Home glucose monitoring
Home glucose monitoring provides a “snapshot” of how your glucose treatment program is doing at one moment in time. This information is particularly important to help you tailor your daily eating program and medication needs to keep glucose in a healthy range. Daily monitoring is vitally important to tell you if the symptoms you are experiencing – sweats, feeling faint, etc. – are the result of a low glucose value (hypoglycemia) so you can treat this problem quickly. Home glucose monitoring is also important when you are sick, or under stress, as it provides you with information you need to make immediate adjustments in your treatment program to keep your blood glucose level in range. By keeping track of glucose levels over a period of weeks, you can begin to see patterns and identify ways in which food, exercise or other factors influence your blood glucose levels. Daily glucose monitoring now comes in many forms by using either a blood glucose monitor or a continuous glucose monitor (CGM). Ask your endocrinologist which method is best suited for you.
Hemoglobin A1c test
While home glucose monitoring is like a snapshot, hemoglobin A1c testing is more like a full length movie – it provides an average view of your glucose level over a period of two to three months. These results will be reported the same day in the laboratory. For people who have not undergone any major changes in their lifestyle or diabetes treatment, hemoglobin A1c tests provide a good assessment of long-term glucose control.
Since A1c is an average, a normal hemoglobin A1c test does not always mean that your glucose has been under control continuously for the past 2-3 months. In fact, since A1c is an average value, sometimes people with swings in blood glucose levels — lots of highs and lows — would also have a normal hemoglobin A1c. This is why daily glucose readings are also important. Dr Noel Somasundaram recommends a target A1c level below 6.5%. If the A1c is above 7% you will need to discuss with your endocrinologist the changes that are required in the treatment plan as well as eating pattern and exercise.
Fructosamine test
The fructosamine test is another measure of glucose control, although it is not as commonly used. The main advantage of the test is that it can detect overall changes in blood glucose control within a few weeks, rather than months. Fructosamine levels indicate the level of glucose control over the past two or three weeks. When changes are being made in your diabetes treatment plan, the Fructosamine test can indicate your level of control over a time span of two weeks.
How to Prevent Heart Disease

Heart disease and diabetes are like twins. A strong link exist between diabetes and heart disease. Those with diabetes have greater risk of heart attacks. Two thirds of the deaths in those with diabetes occurs from heart disease. In fact, cardiovascular disease leading to heart attack, stroke, or peripheral vascular disease leading to amputation are the biggest health risks for those with diabetes.
“For those with diabetes, heart disease can be a serious concern. Cardiovascular disease leading to heart attack or stroke is the No1 cause of death in those with diabetes”, according to Dr Noel Somasundarm, Consultant Endocrinologist.
“There is good-news though: You can take steps to reduce your risk for heart disease”
Dr Noel Somasundarm, MBBS MD FRCP
What are the secrets to minimize your risk of heart disease?
Control your weight. One of the most important things you can do if you have diabetes is maintain a healthy weight. Pay special attention to central obesity- excess weight around the waist area, as it makes you more insulin-resistant. Insulin resistance makes you more susceptible to heart disease. If you are overweight, talk to our dietitian about healthy ways to lose weight.
Get regular physical activity. Regular physical activity has multiple cardiovascular benefits (beyond weight loss). Aim to walk at least 6000 steps a day. Reduce the time you spend sitting. In addition do daily routine physical activity. Start off slowly, and build a plan that works well for you and meets your needs. Regular physical activity makes your heart stronger, enabling it to pump more blood with less effort. Less effort means the force on your arteries decreases. By becoming more active, the systolic blood pressure can be lowered an average of 4 to 9 mmHg. Even if your blood pressure is normal, routine physical activity will prevent high blood pressure from developing.
Don’t smoke. If you already do, make plans to begin a smoking cessation program. Talk to your endocrinologist on how you can be supported to completely give up smoking. It is possible many people quit smoking!. Smoking and diabetes together give you a very high risk of heart disease according to Dr Noel Somadundaram who has helped many people give up smoking completely.
Glucose control. Tight control of glucose can prevent many complications from diabetes and also protects your heart. Aim for an A1C average close to 6.5%, without risking hypoglycemia (low blood glucose). Older adults and those with heart disease may have a more relaxed AIC goal.
Lower your LDL cholesterol (the “bad” cholesterol). Dr Noel Somasundaram recommends an LDL cholesterol goal of less than 70 mg/dl. For this eat healthy- eat more fiber-rich foods, such as fruits, vegetables, and change to whole grain foods. Dr Noel Somasundaram recommends that statin drugs are taken as they have proven in numerous studies to not just lower LDL to goals but reduce heart attacks and death. Routine use of omega-3 fatty acids (fish oil) supplements is not necessary, according to current guidelines. It is best to add at least 2 large pieces (100g each) of fatty fish per week (these include tuna, salmon, mackerel, and sardines in sardine oil) to achieve the need for omega-3 fats.
Control your blood pressure. All people with diabetes should aim for a blood pressure reading of less than 130/80. Limit your daily sodium (salt) intake to <2,300 mg (one teaspoon of salt but remember that all the packaged food contains salt). Too much sodium causes fluid overload and the blood vessels to constrict, which drives up blood pressure.
Insulin
Insulin is the medication used to manage type 1 and, in some cases, type 2 diabetes.
 There are several things you should know about insulin.
There are several things you should know about insulin.
- Insulin is a hormone that lowers glucose in your blood.
- Injected insulin replaces what the body makes naturally. People with type 1 diabetes must take insulin to survive.
- About half the people with type 2 diabetes will need to take insulin at some point in their lives. Taking insulin doesn’t mean you’ve failed; your body may just need extra help.
- Insulin is safe and one of the most effective ways to lower blood glucose. It is measured in units.
Insulin is made in different strengths. Most people use a strength called U-100. - Insulin’s come in several different types. Some are faster-working and last for a shorter period of time while others are slower-working and last for a longer period of time.
- Different companies make different types of insulin. Always use the same brand and type of insulin that your endocrinologist has prescribed.
- Different injection sites (leg, stomach, etc.) may absorb some types of insulin at faster or slower rates.
- The main side effect of insulin is that it can cause hypoglycemia ( low blood glucose levels). Knowing how to recognize and treat lows is an important part of taking insulinTypes of Insulin
All insulin is not the same. The types of insulin differ in: - how fast they begin to work
- when they work their hardest
- how long they continue to work
- how is it being administered
There are two main types and functions of insulin:
Background Insulin (intermediate and long-acting) - Helps control glucose during the night and between meals
- Taken 1-2 times each day
- Background insulins are: NPH (intermediate-acting and cloudy looking), Glargine and detemir insulin (long-acting and clear looking – also called “basal” insulin because they have no peak)Mealtime Insulin (rapid and short-acting)
- Helps control glucose after eating a meal or snack
- Taken before meals
- You may need background insulin, mealtime insulin or both
- Mealtime insulins are: Lispro, aspart, glulisine insulin (rapid-acting and clear looking) and Regular insulin (short-acting and clear looking)
- Premixed Insulin
- Premixed insulin is a combination of background and mealtime insulin.
- Humulin 70/30, Mixtard 30/70, and Wosulin 30/70 are premixed insulins that have some slower-acting (NPH) and some fast-acting (Regular) insulin in one bottle.
- Humalog 75/25, Humalog 50/50, Novomix 30/70 and Novomix 50/50 also contain some slower-acting insulin along with some rapid-acting (lispro and aspart) insulin in one bottle.
Your provider will tell you:
- which brand of insulin to use
- what type or types of insulin to use
- how many units of each type to use
- what time(s) to use insulin each day
Generic Name | Product | When to take | When starts | Works best | How long it lasts | |
Mealtime Insulin | ||||||
Rapid-acting | aspart | Novorapid | 0-15 min before meal | 10-30 min | 30 min - 3 hours | 3-5 hours |
Short-acting | Regular (R) | Humulin R | 30 min before meal | 30-60 min | 2-5 hours | up to 12 hours |
Background Insulin | ||||||
Intermediate-acting | NPH (N) | Humulin N | Does not need to be given with meal | 90 min - 4 hours | 4-12 hours | up to 24 hours |
Long-acting | detemir glargine | Levemir Lantus | Does not need to be given with meal | 45 min - 4 hours | minimal peak | up to 24 hours |
Do you know how to take care of Insulin, Syringes and Pen Needles?
How to store insulin?
Although manufacturers recommend storing your insulin in the refrigerator, injecting cold insulin can make the injection more painful. To counter that, you can store the bottle of insulin you are using at room temperature (27-33ºC) for about one month. You can also carry the insulin with you when you travel for work or holidays this way- in your pocket or in bags. Do not keep bottles in a hot place like near a fire or in direct sunlight. Also, do not keep them near ice or in places where the insulin may freeze. Freezing and too much heat -both destroy the insulin.
If you buy more than one bottle at a time, store the extra bottles in the refrigerator. Then, when needed, take out the bottle ahead of time so it is ready for your next injection. Unopened bottles in the refrigerator are good to last till the expiration date on the packaging.
Do not use insulin after it has been kept at room temperature for longer than one month. Also, do not use insulin past the expiration date printed on the bottle, or if it looks different than usual. Unopened bottles of insulin and unopened insulin pens should be stored in the refrigerator and are good until the expiration date on the packaging.
Examine the bottle closely to make sure the insulin looks normal before you draw the insulin into the syringe. Insulin aspart, lispro, regular, or glargine should be clear and not cloudy. Check for particles or discoloration of the insulin. NPH insulin should look milky and should not be “frosted” or have small particles or clumps in the insulin. If you find any of these in your insulin, do NOT use it.
Syringes
Most people use plastic syringes, which are made to use once and then throw away. Some people use a syringe two to three times. If you reuse a syringe, follow the steps below:
1. Flush the syringe with air to prevent the needle from clogging.
2. Do not wipe the needle with alcohol. This removes the Teflon coating.
3. Recap the needle when not in use.
4. Store the syringe at room temperature.
5. Keep the outside of the syringe clean and dry.
6. Throw away the syringe if the needle is bent or dull or if it has come in contact with any surface other than skin or the top of the insulin bottle.
7. Discard if the calibration lines are difficult to read.
8. Be sure to check your skin around your injection site for unusual redness or signs of infection.
9. Never share syringes.
10. An insulin pen should not be stored with the needle still attached, as this can lead to insulin leakage and air in the cartridge.
How do I dispose of syringes?
Most people injecting insulin with syringes use plastic syringes which are made to be used once and then thrown away. It is not recommended that you re-use syringes. Pen needles should not be reused and should be changed after each use.
It is a good safety practice, and good for the environment, to dispose of syringes and lancets properly. The following are guidelines for proper disposal:
- Dispose immediately after use into a heavy-duty, non-breakable container—one that cannot be punctured—such as a coffee can or detergent container.
- To decrease the chance of another person using your syringe after you dispose of it, separate the plunger from the barrel. Do NOT recap, bend, or break needles.
- When the container is nearly full, it should be covered, taped, and labeled “contaminated”.
Sharps disposal
Each country and town has its own rules for throwing away used needles. Check with local authorities about how to dispose of your “sharps”. Always remember, safety is the best policy.
Nutrition
What can you eat?
It’s all about eating healthy so that you keep illnesses away and live a long and healthy life. The secret is to find the right balance that works for you.
When you’re managing diabetes, your eating plan is a powerful tool. But figuring out what to eat can feel like a hassle. Well, it doesn’t have to- healthy food doesn’t mean boring and tasteless. You can chose healthy options and creative ways to prepare the food with flavor- including healthy twists on your favorite foods.
The one key to feeling your best lies in the food you eat—so don’t give up. You can start by working with our dietitian who will guide you to make an eating plan that works for you. Be sure to include foods you like and don’t be afraid to try be adventurous to find out and explore.
Most importantly, remember that eating well—and adding activity to your daily routine (moving more)—are important ways you can manage diabetes. And we’re here to help you every step of the way.
“What can I eat?” is the important question asked by people with diabetes when they are diagnosed. Everyone’s body responds differently to different types of foods and diets, so there is no single “magic” diet for Diabetes. You can follow a few simple tips and find out what works for you to help manage your blood sugar.
Diet Plans



